Covid vaccine and blood cancer
How to book a covid vaccine if you have blood cancer, or live with someone who does
Find out how many covid vaccinations you should have, and how to get them.
Page updated 11 January 2022
Future vaccine doses in 2023
At the moment we do not know what the plans are for any further covid vaccine doses in 2023. However this is something we are continuing to ask the NHS and government about. We will update our information and social media channels as soon as we know more.
If you haven't had your Autumn booster yet, you can still book that.
Autumn boosters from September 2022
The Autumn booster programme has now started. People should be offered an appointment between September and December, with those at highest risk (including people with blood cancer and their household contacts) being offered their boosters first.
Regardless of how many doses you've had so far, if you haven't had the Autumn booster yet, you can book it now. For people with blood cancer or immunosuppression, this could be up to your sixth dose of the covid vaccine.
When and how can I get an Autumn booster?
In England, from 7 September 2022, people who are immunosuppressed (including people with blood cancer) and their household contacts can book their Autumn covid booster online (or call 119 to book).
Booking your booster appointment online is the easiest way to get one. The NHS has also advised local sites to allow people with a weakened immune system to self-declare and attend walk-ins and vaccination centres, to make getting the extra protection as easy as possible. If you have any letters that show your condition or treatment, it might still be worth taking these with you, but you shouldn't need to provide any evidence this time. The NHS advises that as long as it's been three months since your previous dose, you'll be able to book the Autumn booster.
In Scotland, from 5 September 2022, people who are immunosuppressed and their household contacts will be invited for an Autumn booster by the NHS. You might also want to check the online portal or call the vaccination helpline on 0800 030 8013 if you have any questions.
In Wales, from 1 September 2022, people who are immunosuppressed and their household contacts will be invited for an Autumn booster by their health board.
In Northern Ireland, from 19 September 2022, people who are immunosuppressed and their household contacts can book their Autumn booster online.
Shorten your booster wait
We know some people are worried about attending busy vaccination centres for their covid vaccines. The NHS have sent us this poster, clarifying that you can be fast-tracked if you are immunosuppressed, so you don't have to wait in a busy queue. You may want to print this out and take it to your vaccination centre, to help you ask for the extra protection.
Who can get an Autumn booster?
The following groups should be offered an Autumn booster in 2022:
- all adults aged 50 years and over
- people aged 5 to 49 years in a clinical risk group (including people with immunosuppression)
- people aged 5 to 49 years who are household contacts of people with immunosuppression
- people aged 16 to 49 years who are carers
- residents in a care home for older adults and staff working in care homes for older adults
- frontline health and social care workers
We've produced this document with the British Society for Haematology to help improve awareness of the Autumn booster among healthcare professionals:
Which vaccine will I get?
The Autumn booster roll-out will primarily use the next generation, bivalent covid vaccine, which targets both the original strain of coronavirus and the Omicron variant.
Moderna's bivalent vaccine was approved as a booster in the UK on 15 August 2022. It is an mRNA vaccine. It targets both the original strain of coronavirus (called 'wild type' or original strain) and the first Omicron variant (called Omicron BA.1).
In this bivalent vaccine, half of the vaccine targets the original virus strain, and the other half targets Omicron. Clinical trials showed that this booster triggered a strong immune response against both Omicron (BA.1) and the original strain of coronavirus. It might also generate a good response against Omicron sub-variants BA.4 and BA.5.
Pfizer has also made a bivalent vaccine which was approved as a booster on 3 September 2022. Similar to the Moderna bivalent vaccine, half of the vaccine targets the original virus strain and half of the vaccine targets Omicron BA.1.
These combination vaccines, like all other vaccines, have been approved because they've been tested and found to be safe and effective.
Previous vaccines are also still highly effective, so if you are not offered a new bivalent vaccine, don't hesitate to take the vaccine you are offered. Getting a vaccine quickly is much more important in terms of protecting you, rather than which type of vaccine you get.
Why should people with blood cancer have another vaccine dose?
People with blood cancer do not respond as well to vaccinations as the rest of the population. This is because for a vaccination to work, your immune system needs to react, and if you have blood cancer, your immune system might not work quite as well.
But, studies have shown that even if people don't generate covid antibodies after their first few covid vaccine doses, they can go on to develop antibodies after more doses. Having multiple covid vaccine doses gives you the best chance of protecting yourself from covid, which we know is a serious risk to people with blood cancer.
In particular this year, many more people are mixing now than in previous winters, so it's vital to protect yourself against flu and covid with the latest vaccine doses.
Flu jabs
Depending on supply, you might be offered your flu vaccination at the same time as your covid booster. It's really important to get your flu jab if you have blood cancer. Data shows that having both jabs on the same day is safe and doesn't reduce the effectiveness of either vaccine. The earlier you get both jabs, the more protected you will be going into autumn/winter.
If you currently have any type of blood cancer, whether you are having treatment or not, you should get a free priority flu jab. If you had blood cancer in the past, but you still have a compromised immune system, then you should also get a free priority flu jab.
There's a range of flu jabs available for the 2022-2023 season. People in different age groups or at different levels of risk may be given different vaccines - the one you're offered will be one that's suitable for you. You can ask the person giving it to you which one you're having and why.
For a child aged 16 or under who has blood cancer or a compromised immune system, they should not get the nasal spray version of the flu vaccine, as this is a live vaccine. They should have the jab version instead, which is not live.
Evusheld made available privately in the UK
A preventative treatment called Evusheld has been made available privately in the UK. Evusheld is an antibody treatment that can be used to prevent people with blood cancer getting covid in the first place. Find out more about accessing Evusheld privately, and how we are lobbying for free access.

Spring boosters from April 2022
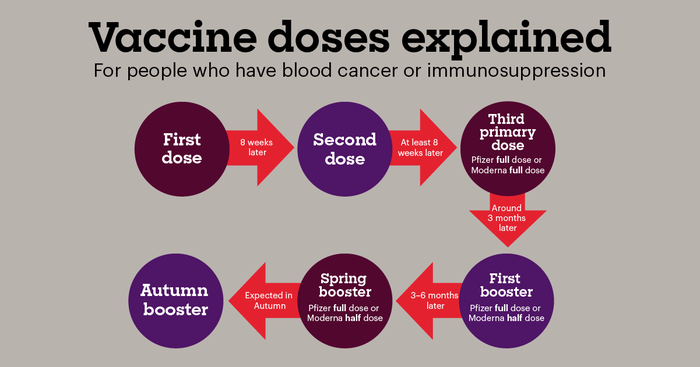
Anyone aged 12+ with blood cancer or immunosuppression should have had another booster dose of the vaccine in Spring 2022. This should have been your fifth vaccine dose. The covid vaccine schedule for blood cancer patients to this point was:
- 1st primary dose – from around Jan 2021
- 2nd primary dose – from around April 2021
- 3rd primary dose – from around September 2021
- 4th dose (1st booster) – from around January 2022
- 5th dose (Spring booster) – from around April 2022
- 6th dose (Autumn booster) – expected September 2022
Regardless of which doses you've had so far, you should now get your Autumn booster - see above.
Most people who are living with blood cancer and many who are in remission from blood cancer have a weakened immune system, which makes it harder to fight off viruses and other bugs. This is called immunosuppression. Immunosuppressed people are at higher risk of getting seriously ill from covid.
That's why, when covid vaccines first become available, people were prioritised for vaccination if they:
- had any type of blood cancer (leukaemia, lymphoma, myeloma, MDS, MPN), whether they were on treatment or not
- were immunosuppressed as a result of blood cancer in the past
- had had a stem cell or bone marrow transplant in the past
- had any other underlying condition that meant they were classed as "clinically vulnerable" or "clinically extremely vulnerable".
Because immunosuppressed people are at higher risk from covid, household contacts (people who live most of the time with someone who is immunosuppressed) and unpaid carers were also prioritised for vaccination.
Going forward, people who are immunosuppressed, including most people with blood cancer, are being offered extra vaccinations. While covid vaccinations may not work as well for immunosuppressed people, there's evidence that repeated doses can offer better protection. People who are severely immunosuppressed may also be eligible for new antiviral treatments if they get covid.
We have more information about research into how effective covid vaccinations are for people with blood cancer.
Ask the Experts
Watch our ‘Ask the Experts’ session about additional vaccine doses, ongoing research and upcoming treatments. Featuring Professor Emma Morris (leading a vaccine effectiveness study), Dr Alison Uriel (working on a trial for alternative methods of protection from covid), Dr Maggie Wearmouth (from the Joint Committee for Vaccination and Immunisation), Claire Amaladoss (Deputy Director of the Vaccine Deployment Strategy at NHS England) and Rachel Kahn (Research Communications Manager at Blood Cancer UK).
Who should have a third primary dose?
The third primary dose is for people who had weakened immune systems at the time of their first or second vaccination, who might not have produced enough antibodies from the vaccine. This includes anyone with blood cancer or ongoing immunosuppression. The third primary dose aims to increase the level of protection gained from the vaccine.
People who get a third primary dose of the vaccine will also be offered a booster (fourth dose) 3 months after their third dose.
The group offered a third primary dose includes people who:
- were having treatment for blood cancer, or were in remission after having treatment in the previous 12 months
- had either an allogeneic or autologous stem cell transplant in the previous 24 months
- had a stem cell transplant more than 24 months before, but had ongoing immunity issues
- were on watch and wait (active monitoring) for any type of blood cancer.
We've been assured that there is room for clinical judgement on who gets the third primary dose. So groups that aren't specifically mentioned in the guidance but are considered to be at high risk can get a third dose. This means people who were in remission for longer than 12 months when they had their previous vaccinations will be eligible if their GP or hospital team recommend it.
If you're currently having treatment, your treating team should advise you about the best timing for your third dose.
How will the effectiveness of the third primary dose be monitored in people with blood cancer?
The efficacy of the third dose will be monitored by the OCTAVE DUO study, explained on our vaccine efficacy research page.
Research is also going on to find other ways to prevent and treat coronavirus for people who don't get full protection from covid vaccines.
Flu vaccines and covid vaccines
We've had some calls from people asking whether they need to leave a gap between their flu jab and their covid vaccine. This isn't necessary, and it's really important you get your flu jab, so please take it as soon as you're offered it.
When covid vaccines were first rolled out in early 2021, the guidance said not to have a flu jab within 7 days of the covid vaccine. However, this advice has now changed, as we have the data to show it's safe to have them together. You might want to show this web page to your GP.
The MHRA have confirmed that data from the ComFluCOV trial shows that having both jabs on the same day is safe and doesn't reduce the effectiveness of either vaccine. The NHS also confirms this, saying 'Some people may be eligible for both the flu and the covid-19 booster vaccines. If you are offered both vaccines, it's safe to have them at the same time.'
Getting protected against flu and covid is really important for people with blood cancer, so if you're offered either vaccine, do take them. If they are close together or even on the same day, this is fine.
Flu vaccines for adults and children
If you currently have any type of blood cancer, whether you are having treatment or not, you should get a free priority flu jab. If you had blood cancer in the past, but you still have a compromised immune system, then you should also get a free priority flu jab.
You might be offered the flu jab at the same time as your third covid vaccine dose.
For 2021, the JCVI have recommended that countries in the UK offer free flu jabs to all of the following groups:
- all children aged 2 to 15 by 31 August 2021 (but not 16 years or older) (nasal spray version)
- those aged 6 months to under 50 years in clinical risk groups
- pregnant women
- those aged 50 years and over
- those in long-stay residential care homes
- carers
- close contacts of immunocompromised individuals
- frontline health and social care staff
For a child aged 16 or under who has blood cancer or a compromised immune system, they should not get the nasal spray version of the vaccine, as this is a live vaccine. They should have the jab version instead, which is not live.
People aged 16 to 64 years with underlying health conditions
If you are under 65, and you're not already included in priority group 4 (clinically extremely vulnerable), then you are in group 6 if you have had a stem cell or bone marrow transplant in the past, if you have immunosuppression due to disease or treatment, or if you have any other underlying conditions listed in the government's guidance under 'Persons with underlying health conditions'.
The government refers to The Green Book for a definition of 'immunosuppression' and The Green Book defines "anyone with a history of haematological malignancy" as immunosuppressed - see Chapter 14a page 11 of The Green Book. So if you have a history of blood cancer, you could be in priority group 6.
Although the government guidance automatically puts people whose stem cell transplant was over 6 months ago in priority group 6, it also highlights that clinicians will use their judgement to add other people to priority group 4 if they feel that's best. If you've had a transplant in the past, we have more information and sources to help you talk to your doctor about which group you are in.
If you are in priority group 6, your GP will need to know this in order to invite you for a vaccine or allow you to book it online. Try the links and numbers at the top of this page to book your vaccine, and if this doesn't work, contact your GP.
Unpaid carers (if you look after someone with blood cancer)
Unpaid carers are people who are the main carer of an elderly or disabled person (adult or child – and cancer counts as a disability) whose welfare may be at risk if the carer falls ill, or anyone who is eligible for Carer’s Allowance.
If you think you may be an unpaid carer but aren't on Carer's Allowance, read this information from Carer's UK, and contact your GP to register as a carer.
Ideally, you should be registered as a carer to get the vaccine in group 6. You can tell your GP you are a carer, even if you don't qualify for or get Carer's Allowance.
In Scotland, you should still let your GP and/or local carer centre know you are an unpaid carer, but in terms of getting the vaccine, you will also need to self-refer for the vaccine.
We are aware that people who live with someone with blood cancer have been able to get a vaccine by various methods:
- First try the links and numbers for your country at the top of this page.
- Call or email your GP to tell them you're looking after someone with blood cancer.
- Call 119 and tell them you're looking after someone with blood cancer.
- Contact your local vaccination centre and tell them you're looking after someone with blood cancer.
Household contacts of immunosuppressed people (if you live with someone with blood cancer)
On 29 March 2021, the JCVI recommended that household contacts of people who are severely immunosuppressed get a covid vaccine in priority group 6, along with unpaid carers and people with underlying health conditions.
As of 27 April 2021, we are aware that the NHS in England, Scotland and Wales are following this advice. We are awaiting confirmation from Northern Ireland as to whether they will also follow it.
Anyone who is a household contact of someone with a history of blood cancer should now be offered a covid vaccine in England, Scotland and Wales.
If you need help talking to your GP about getting the vaccine as a household contact of someone with blood cancer, share the below document with them. This document currently refers to England, but it may be helpful for people in Scotland and Wales too. We will update it for Scotland and Wales as soon as the NHS in those countries releases guidance on how they will implement the vaccines for household contacts.
Household contacts are adults who expect to share living accommodation on most days with someone severely immunosuppressed, where continuing close contact is unavoidable. Both the immunosuppressed person and the household contact need to be 16 or over. Members of support bubbles who do not share living space with the person for the majority of the week are excluded from the definition, but they may be eligible for vaccination in group 6 as registered or unpaid carers (see above).
'Severely immunosuppressed' is defined by the JCVI (and The Green Book on page 11) as:
- anyone with a history of haematological malignancy - this means anyone with a history of blood cancer
- people who require long-term immunosuppressive treatments
- people who are receiving immunosuppressive or immunomodulating biological therapy, or steroid sparing agents
- people treated with or likely to be treated with systemic steroids for more than a month at a dose equivalent to prednisolone at 20mg or more per day for adults.
You can see the letter sent to GPs in England, the update from the government in Wales, the web page from the NHS in Scotland which mentions household contacts, and also the letter from the JCVI, and the letter from Matt Hancock.
Guidance in England:
GPs will write to any patients they have who are immunosuppressed to tell them about this.
If you are a household contact of someone with a history of blood cancer, you should contact your GP to book a vaccine.
You will need to take your own proof of address to your vaccination, which matches the address of the immunosuppressed person, although GPs have been asked to be flexible if in some situations you are a close contact that does not live at the same address.
If you are registered at a different GP to the immunosuppressed person, you can use the letter they receive with your own GP to book your vaccine.
If household contacts have trouble booking their vaccination
We’re hearing that a few GPs in England aren't aware that household contacts are now eligible for vaccination, or aren't aware that appointments should be booked through them. If you're a household contact and this happens to you, show your GP the letter we've prepared above. The guidance from NHS England states very clearly that household contacts are eligible and that vaccinations should be arranged through the GP surgery.
If you need to take things further, you can ask to speak to the Practice Manager at your surgery and if necessary, make a complaint. Or contact the customer contact centre for NHS England.
We're aware that some household contacts aged 16 to 18 are finding it difficult to get vaccinated because of low supplies of the Pfizer vaccine - the only one approved for this age group. If this happens, follow the advice above under "If your second vaccination appointment is cancelled".
For Scotland and Wales, we don't yet know what the process for booking household members' vaccinations will be - we will update this page when the guidance is published.
Which people with blood cancer are on the Shielded Patients List?
Blood cancer affects the immune system, and so do its treatments.
Adults with blood cancer may have a compromised immune system and therefore be at high risk of serious illness from coronavirus.
Even people who are not on treatment (for example, those on ‘watch and wait’) may have compromised immune systems due to the cancer itself.
Since the start of the pandemic, we have learned more about how coronavirus affects different people, and it is clear that people with blood cancer have a higher chance of getting seriously ill from coronavirus and of dying with it. A recent meta-analysis of studies found that 34% of people with blood cancer in hospital with coronavirus died.
It is crucial that people with blood cancer who are clinically extremely vulnerable are on the Shielded Patients List so they are invited for their vaccine at the appropriate time.
Being on the Shielded Patients List also means people will receive relevant letters from the Department of Health & Social Care. In some areas where the risk is very high, the government are advising this group not to go out to work, and these letters provide evidence to people’s employers and enable them to access sick pay and other government support.
The government automatically includes adults with blood cancer in the clinically extremely vulnerable group if they:
- are having chemotherapy, immunotherapy, other antibody treatments, or targeted treatments that affect the immune system (eg protein kinase inhibitors/TKIs)
- currently have any type of blood cancer (this includes leukaemia, lymphoma, myeloma, myelodysplastic syndromes, myeloproliferative neoplasms, including essential thrombocythaemia (ET), polycythaemia vera (PV) and myelofibrosis (MF)), whether they’re on treatment or not, including people on watch and wait.
- are on immunosuppression medication after a transplant, have GvHD, or have ongoing immunodeficiency after a transplant
- have had a stem cell transplant in the last 6 months*
*If your transplant was more than 6 months ago, the government automatically classes you as vulnerable (not extremely vulnerable). But – your doctor can choose to move you to the extremely vulnerable group. We have more information and sources to help you talk to your doctor about which group you are in.
In England, the Clinical Director for Cancer (Peter Johnson) sent a letter to all cancer teams, with added clarification that the high-risk criteria includes blood cancer patients:
- before, during or after treatment, including those being managed expectantly (on watch and wait)
Chronic myeloid leukaemia (CML) and Myeloproliferative neoplasms (polycythaemia vera, essential thrombocythaemia, myelofibrosis)
There has been some uncertainty about how high-risk CML and MPN patients are. The NHS at a national level does include all CML and MPN patients in the clinically extremely vulnerable category.
Now that we know how high-risk blood cancer patients are from coronavirus, it is crucial that all blood cancer patients, including CML and MPN patients, are added to the Shielded Patients List (listed as clinically extremely vulnerable) and invited for their covid vaccine as part of priority group 4.
A recent meta-analysis of studies found that 34% of people with MPNs and CML in hospital with coronavirus died.
GPs can and should add their CML and MPN patients to the Shielded Patients List. This could be important for the future, for example for future covid vaccine roll-outs, or government support for those shielding.
MPN Voice has this statement on its website, clarifying that MPN patients should be offered the vaccine.
The International Chronic Myeloid Leukaemia Foundation (iCMLf) has this statement on its website, clarifying that CML patients should be offered the vaccine.
If you have an MPN and are having trouble getting on the shielding list, share this document with your GP. It explains why you should be on the list and how to add you:
Are people in remission from blood cancer clinically extremely vulnerable?
Patients in remission from myeloma could still have a compromised immune system and are included in the criteria as someone who "currently has any type of blood cancer”. They should be on the Shielded Patient List.
Patients in remission with a chronic blood cancer could still have a compromised immune system and are included in the criteria above as someone who "currently has any type of blood cancer”. They should be on the Shielded Patient List unless their specialist doctor advises otherwise.
Patients in remission from any other blood cancer: The length of time it takes for the immune system to recover after cancer and its treatment varies depending on the type of cancer, the treatment given and the person as an individual. There is no specific time frame. Generally, it takes a few months to a year to recover. Many people’s immune systems recover to a normal level after treatment. However, some patients experience ongoing issues with being more prone to infections and getting more severe infections. It’s important to discuss this with patients and their specialist blood cancer teams, to agree whether they would benefit from being on the Shielded Patients List. Even if they are not on the shielding list, they may still be 'clinically vulnerable' (rather than clinically extremely vulnerable) and should therefore be included in priority group 6 for the covid vaccine - see above under 'People aged 16 to 64 years with underlying health conditions'.
Patients who finished chemotherapy in the last 3 months: These patients may still have a compromised immune system. This should be discussed with the patient’s specialist blood cancer team.
Patients who've had a stem cell transplant: If the transplant was in the last 6 months, they are automatically classed as clinically extremely vulnerable and should be on the Shielded Patient List. If the transplant was over 6 months ago, the government guidance automatically classes them as vulnerable (not extremely vulnerable). But – their doctor can choose to move them to the extremely vulnerable group if they feel this is best. We have more information and sources about how long people may be extremely vulnerable for after a transplant.
Support for GPs
If you have any patients affected by blood cancer, you can signpost them to Blood Cancer UK for support and information.
We are also very happy to speak to GPs and other healthcare professionals if helpful - contact us for information about blood cancer and coronavirus.
Our support line offers emotional and practical support. It is free to call on 0808 2080 888 or email support@bloodcancer.org.uk
Our website has up-to-date information about blood cancer, coronavirus, and living with blood cancer.
Where can I have the covid vaccine safely?
The covid vaccine will be rolled out at hospital hubs, local community services (like GP surgeries), and vaccination centres (like conference centres and sports stadiums).
Any setting administering the vaccine will follow strict guidelines to ensure this is a COVID-safe environment for clinically extremely vulnerable people to visit.
GPs and any other settings delivering coronavirus vaccines have been given strict guidelines and instructions on things like:
- storage and handling of the vaccine
- training of healthcare providers who will administer the vaccine
- ensuring a COVID-safe environment
- managing side effects and any reactions
- monitoring patients when they have the vaccine and for 15 minutes afterwards.
They have also had their site inspected to ensure they are ready for the roll-out.
What are the side effects of the covid vaccine?
Like all vaccines, the Pfizer, AstraZeneca/Oxford and Moderna covid vaccines can cause side effects, although not everybody gets them.
Pfizer vaccine side effects
Most side effects are mild or moderate and go away within a few days.
Common side effects include pain, swelling or redness at the injection site, tiredness, headache, muscle pain, chills, joint pain, fever and nausea (feeling sick).
Here is the full list of reported side effects, including less common ones: Pfizer vaccine side effects.
AstraZeneca/Oxford vaccine side effects
Most side effects are mild or moderate and go away within a few days, with some still present a week after vaccination.
Common side effects include tenderness, pain, warmth, redness, itching, swelling, bruising or a lump where the injection is given, generally feeling unwell, feeling tired (fatigue), chills or feeling feverish, fever, headache, feeling sick (nausea), being sick (vomiting), joint pain or muscle ache, and flu-like symptoms, such as high temperature, sore throat, runny nose, cough and chills.
Here is the full list of reported side effects, including less common ones: AstraZeneca/Oxford vaccine side effects.
Moderna vaccine side effects
Most side effects go away within a few days of appearing.
Common side effects include tenderness and swelling of the underarm glands on the same side as the injection site, pain or swelling at the injection site, headache, nausea (feeling sick), vomiting, muscle ache, joint aches, stiffness, feeling very tired, chills and fever.
Here is the full list of reported side effects, including less common ones: Moderna vaccine side effects.
Healthcare workers who administer the vaccine can tell you about any side effects and are trained in what to watch out for. You will also be asked to wait for 15 minutes after your injection to make sure you are OK before you leave.
Join our mailing list for key updates about coronavirus for people with blood cancer, what we're doing to help, and ways you can help, including campaigns you may be interested in.
Support for you
Call our free and confidential support line on 0808 2080 888. We are currently receiving a very high volume of calls related to coronavirus, so if you're not able to get through straight away, please leave a message and we'll get back to you as soon as we can.
You can also email us if you prefer to get in contact that way. We'll usually get back to you within two working days, but due to the current rate of calls and emails we are currently receiving it may take us longer.
Talk to other people with blood cancer on our Online Community Forum – there is a group for coronavirus questions and support.
You can also find out what's helping other people affected by blood cancer through coronavirus and beyond in our pages on living well with or after blood cancer.
The following companies have provided funding for our coronavirus support, but have had no further input: AbbVie, AstraZeneca, Celgene, Gilead, Incyte, Kyowa Kirin, Novartis, Pfizer, Sanofi, Takeda.

